The words “stem cell research
and therapy” evoke a number of responses. In emotionally vulnerable patients, a
sense of hope. In scientists, a great deal of excitement about future
prospects. In the case of legal experts and ethicists, a need to ensure that
patient safety and a spirit of distributive justice are maintained. And in the
minds of entrepreneurs, an opportunity to develop a profitable business.
Stem cells are the building
blocks of our bodies. They are able to differentiate into the more that 200
cell types that make up our bodies. From a fertilised egg to a fully-fledged
human being which contains billions of cells, the purpose of stem cells during
development in the womb is to ensure normal structure and function.
In postnatal life, stem cells
replace those cells that have been damaged by wear and tear or by disease.
Gaining Momentum
In research, stem cells are at
the cutting edge of science, with regular breakthroughs being announced in the
field. By 2012, it was estimated that there were close to 100,000 active stem
cell researchers across the globe. Massive funding is being directed globally
into research which continues to provide hope to millions of patients.
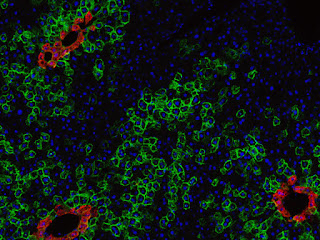
Stem cell therapy translates
the research findings into potential cures for many diseases. For instance, for
more than 50 years, bone marrow transplants – also known as hematopoietic stem
cell transplants – have been used to treat patients with blood cancers such as
leukemia and blood disorders such as sickle cell disease and thalassemia.
When a person with cancer
undergoes conditioning chemotherapy to destroy the cancerous cells in the body,
in the process this treatment also destroys the patient’s own stem cells. Bone
marrow transplants are used to replace these stem cells. This form of treatment
is universally employed, and accepted.
More recently, skin grown from
stem cells has been used to treat extensive burns and stem cells from fat
(adipose tissue) have been used as tissue fillers.
The reality of stem cells versus future promise
Stem cell treatment has saved
many lives. But there are also elements of stem cells that have been mired in
controversy.
As a result of stem cells
becoming a buzzword, there has been a proliferation of websites offering
dubious treatments, luring people with incurable diseases who are emotionally
vulnerable. There is rarely any form of control over what these clinics place
on their websites, let alone the treatments they offer.
Aside from bone marrow
transplants and stem cells used for burns, almost all other conditions for
which stem cells are advertised to provide a cure are still in an experimental
stage. Globally, there are hundreds of legitimate clinical trials underway to
assess the effect of stem cells in a variety of conditions including heart
disease, spinal cord injury, blindness and Parkinson’s disease, to name a few.
But, in these cases, the road
which finally joins the healing properties of stem cells to the approved use of
these cells on a routine basis is long and arduous.
Clinical trials need to be
undertaken before a treatment can become part of routine medical practice. They
must be registered with the relevant national body in the country where they
are taking place. Clinical trials also need to be peer reviewed via a registered
ethics committee or an institutional review board.
And although rarely mentioned
explicitly in legislation or guidelines, patients who receive experimental
treatments should not have to pay for these treatments.
Breaching The Law On Multiple Fronts
For most stem cell treatments
which have not undergone clinical trials, patients are subjected to therapy
which defies the basic ethical and legal principles of the medical profession.
Some treatments are blatantly unsafe, such as the infusion of embryonic and
animal-derived stem cells into humans.
But practitioners who provide
these unproven treatments argue that:
patients are desperate and it
is a last resort after trying everything else;
If one uses the patient’s own
cells the rules do not apply; and
patients should have the right
to decide how they wish to use their cells.
Countries without adequate
legislation cannot curb unethical practices and financial exploitation of
patients using unproven stem cell treatments. In these countries, unscrupulous
medical practitioners providing these therapies often identify the gaps in the
law and then head straight for them, using legal tactics and devious
interpretations to justify their activities.
Regulating Stem Cell Treatment
To ensure the safety of stem
cell treatments and to limit exploitation of vulnerable patients, several
measures can be undertaken. These include establishing appropriate legislation,
ensuring that this legislation is enforced, and educating the public.
Ethical advertising standards
also need to be enforced to limit the dissemination of false information. And
patients should feel they have the freedom to approach their medical
practitioners for advice on how to proceed.
Without an adequate
legislative environment or the enforcement of existing legislation, the medical
industry is at risk of facing legal challenges from unsatisfied or damaged
patients. This is likely to slow down advances in the field, although it will
also provide much needed case law which, due to the relative youth of the
field, is still lacking in many countries, including South Africa.
But the outcome could also
include a knee-jerk reaction that results in excessively prescriptive
legislation that limits research on valuable ethically and scientifically
approved projects as well as the translation of research findings into useful
products and services.
Source : http://goo.gl/rv7vbI